People with sickle‑cell disease face a stroke risk that’s several times higher than the general population—often striking without warning. Understanding the why, how, and what you can do today can literally protect the most precious organ you have: your brain.
In the next few minutes we’ll walk through the science, the screening tools, the newest treatments, and the everyday steps that keep blood flowing smoothly. Think of this as a friendly chat over coffee, not a textbook.
Why Stroke Happens
How sickled cells block blood flow
Sickle‑cell disease (SCD) is caused by a mutation in the hemoglobin‑β gene that turns normal, round red blood cells into rigid, crescent‑shaped “sickles.” These misshapen cells can’t squeeze through tiny capillaries, so they get stuck, depriving tissues of oxygen. When this happens in the brain’s arteries, the result is an ischemic stroke.
Numbers that matter
According to the CDC, about 10 % of children and up to 24 % of adults living with SCD will experience a symptomatic stroke. Silent strokes—brain lesions that show up on MRI but cause no obvious symptoms—affect 20‑40 % of children and more than half of adults.1
Sickle‑cell trait vs. disease
Carrying just one copy of the abnormal gene (sickle‑cell trait, SCT) does increase risk, but only modestly. The ARIC study found a 1.4‑fold higher hazard of ischemic stroke in African‑American carriers compared with non‑carriers.2 In contrast, full‑blown SCD carries a risk that is dozens of times higher.
| Condition | Gene status | Typical stroke risk | Key study |
|---|---|---|---|
| Sickle‑Cell Disease (SS or Sβ⁰) | Two abnormal β‑globin copies | 5‑10 % (children) → 24 % (age 45) | STOP trial 1998; H&O 2025 |
| Sickle‑Cell Trait (heterozygous) | One abnormal copy | HR ≈ 1.4; +1.9/1,000 person‑years | ARIC 2014; 30‑year risk 2019 |
Types of strokes in SCD
Children most often suffer ischemic strokes caused by vessel narrowing, while adults between 20‑29 years are more prone to hemorrhagic strokes. Both types are linked to the same underlying problem: sickled cells irritating the vessel lining, prompting clot formation or vessel rupture.
How Doctors Measure Risk
Transcranial Doppler (TCD) screening
The frontline tool is the transcranial Doppler ultrasound. It measures blood‑flow velocity in the major arteries of the circle of Willis. A velocity over 200 cm/sec (or >190 cm/sec in some protocols) flags a child as high‑risk, prompting preventive treatment.
Annual TCD scans are recommended for every child with SCD from age 2 to 16 years.3 The test is painless, takes about 20 minutes, and feels like a gentle head massage.
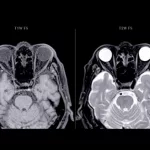
MRI for silent strokes
Even if a child never shows obvious symptoms, an MRI can reveal “silent” infarcts—tiny lesions that silently erode cognitive function over time. Detecting these early helps doctors adjust therapy before problems surface.
Blood‑work clues
Low hemoglobin, high white‑cell counts, and especially chronic kidney disease (CKD) amplify stroke risk. A 30‑year ARIC analysis showed CKD triples the odds of stroke in carriers of the sickle trait.4
Risk‑calculator tools
Some hospitals offer online calculators that combine TCD results, hemoglobin level, and comorbidities to give a personalized risk score. Ask your hematology team if such a tool is available at your clinic.
Ways to Lower Risk
Chronic blood‑transfusion therapy
Regular transfusions dilute sickled cells with healthy donor cells, lowering the proportion of “bad” red blood cells to under 30 %. The landmark STOP trial demonstrated a 92 % reduction in overt strokes when transfusions were started after a high TCD reading.5 The downside? Iron overload, which requires chelation medication.
Hydroxyurea
Hydroxyurea boosts fetal hemoglobin (HbF), which keeps red cells more flexible. Many patients see fewer pain crises, lower TCD velocities, and a modest drop in stroke incidence. It’s taken orally once a day, making it a convenient outpatient option.
Gene‑therapy breakthroughs
In the last few years, gene‑editing (CRISPR‑Cas9) and lentiviral vector therapies have moved from trials to early‑access programs. Recent gene therapy benefits data show a 60‑80 % reduction in vaso‑occlusive events and a striking decline in new strokes. While long‑term safety is still being tracked, these results are a beacon of hope for families who have watched the disease wreak havoc.
Lifestyle & preventive care
- Stay well‑hydrated—aim for 2‑3 L of water daily, especially in hot weather.
- Control blood pressure and cholesterol; both accelerate arterial damage.
- Avoid extreme temperatures; sudden cold or heat can trigger sickling.
- Maintain a healthy weight and engage in moderate exercise—walking, swimming, or light biking keep circulation lively.
- Manage comorbidities such as CKD, diabetes, or atrial fibrillation; they each add a layer of stroke risk.
Emerging brain‑ischemia treatments
If a stroke does occur, time is brain. New neuroprotective agents and clot‑busting protocols are being refined. For more on the newest options, see our article on brain ischemia treatment.
Spotting a Stroke Fast
FAST + “Feel” for sickle‑cell patients
Everyone knows the FAST mnemonic (Face drooping, Arm weakness, Speech difficulty, Time to call 911). For those with SCD, add a “Feel” step: sudden, severe headache without a clear cause or new, unexplained dizziness. These clues can signal a silent or “cryptic” stroke that needs immediate imaging.
What to say on the phone
When you call emergency services, mention:
- Your diagnosis (e.g., “I have sickle‑cell disease, genotype SS.”)
- Last transfusion or hydroxyurea dose.
- Any recent TCD results, if known.
Providing this context helps paramedics prioritize neuro‑imaging when you reach the hospital.
Post‑stroke care checklist
- Immediate MRI or CT to confirm stroke type.
- Begin appropriate therapy (thrombolysis for ischemic, blood‑pressure control for hemorrhagic).
- Re‑evaluate TCD velocity; often it rises after an event.
- Schedule a follow‑up with your hematologist within 48 hours.
- Consider starting or intensifying transfusion or hydroxyurea therapy, if not already in place.
Living With Confidence
Build a support network
Living with SCD is a team sport. Connect with local Sickle Cell Disease Associations, online forums, and your clinic’s social‑work department. Sharing stories—like the teen who avoided a second stroke after switching to hydroxyurea—reminds us that progress is possible.
Keep a personal health diary
Jot down daily hydration, pain episodes, medication doses, and any changes in vision or cognition. A simple spreadsheet becomes a powerful tool when you discuss trends with your doctor.
Stay informed with clinical research
Clinical trial results are reshaping the landscape of SCD care. A quick visit to clinical trial results keeps you aware of upcoming therapies, eligibility criteria, and enrollment sites near you.
Ask about gene‑therapy options
If you’ve heard the buzz about “gene editing cures,” ask your hematologist whether you qualify for an ongoing trial. The process usually involves a brief screening, a one‑time infusion of modified cells, and a period of monitoring. It’s a life‑changing conversation worth having.
Regular blood‑flow improvement checks
Even when you’re feeling fine, annual gene therapy sickle cell updates, TCD scans, and MRI reviews keep the bloodstream clear. Think of it as a routine oil change for your engine—preventive maintenance beats emergency repairs every time.
Take the First Step Today
We’ve covered the science, the screening, the modern treatments, and the everyday habits that together shrink the odds of a stroke. The most empowering move is to turn this knowledge into action: schedule that TCD, talk to your doctor about hydroxyurea or transfusion options, stay hydrated, and keep an eye on emerging gene‑therapy trials.
If anything feels overwhelming, remember you’re not alone. Every parent, teen, and adult walking this path has faced the same questions—and many have emerged with healthier brains and brighter futures.
What’s the next step you’ll take? Reach out to your care team, start a health journal, or simply share this article with a friend who needs reassurance. Together, we can turn “risk” into “resilience.”





















Leave a Reply
You must be logged in to post a comment.