Hey there, friend. If you’ve ever woken up feeling exhausted, noticed a stubborn belly‑fat pattern, or wondered why your doctor mentioned “elevated liver enzymes,” you might be sitting at the crossroads of two surprisingly connected health issues: sleep apnea and fatty liver. In this post I’m going to unpack the science, share real‑life stories, and give you a clear game plan—so you can stop guessing and start taking action.
Quick Answer
Short and sweet: yes, sleep apnea can make fatty liver (now called MASLD) worse. The link isn’t just the fact that both conditions love a good dose of extra weight. Intermittent drops in oxygen during sleep set off a cascade of inflammation, insulin resistance, and oxidative stress that directly harms liver cells. The good news? Treating the breathing problem and tweaking a few lifestyle habits can pause—or even reverse—this damage.
Yes, It Makes It Worse
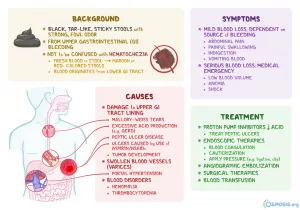
Studies from 2023 and 2024 show that people with moderate‑to‑severe obstructive sleep apnea (OSA) have higher rates of advanced MASLD, including fibrosis (scarring). One Healthline summary notes that the repeated oxygen dips trigger chronic inflammation that fuels liver fat accumulation.
Why It Happens
The body isn’t a set of isolated parts; everything talks to everything else. When you stop breathing for a few seconds at night, your blood oxygen dips, your sympathetic nervous system revs up, and a flood of stress hormones and free radicals pours into circulation. Those molecules love to crash liver cells, making them store more fat and scar over time.
How They Interact
Intermittent Hypoxia
Think of intermittent hypoxia (IH) as a roller‑coaster for your cells. Each dip in oxygen is a brief “panic” moment that forces the liver to work harder, producing reactive oxygen species (ROS). Over weeks and months those ROS become a chronic nuisance, eroding cell membranes and prompting the liver to lay down fibrous tissue.
Study Highlights
A 2023 review described IH as “the most important factor linking OSA and NAFLD.” Researchers measured higher levels of oxidative markers in patients with severe OSA, and those same patients had worse steatosis on ultrasound.
Systemic Inflammation
When you’re gasping for air at night, you also trigger a low‑grade inflammatory response—think of it as the body’s fire alarm constantly being pulled. Cytokines like TNF‑α and IL‑6 rise, and they don’t just sit in the lungs; they circulate and inflame the liver, worsening fatty infiltration.
Real Data
In a 2024 cohort, C‑reactive protein (CRP) levels were 30 % higher in OSA patients with MASLD compared to those with only one condition, underscoring the inflammatory bridge.
Insulin Resistance
Both sleep apnea and fatty liver love insulin resistance. The night‑time oxygen swings mess with glucose metabolism, making cells less responsive to insulin. That pushes more sugar into the bloodstream, encouraging the liver to dump excess calories as fat.
Numbers That Matter
One analysis showed a 1.8‑fold increase in HOMA‑IR (a measure of insulin resistance) among people with an apnea‑hypopnea index (AHI) above 30, compared with those under 5.
Oxidative Stress
Imagine your liver as a delicate kitchen; oxidative stress is like a constant drizzle of hot oil that burns the surfaces. Repeated oxygen shortages create free radicals that damage mitochondria—the power plants of liver cells—leading to cell death and scarring.
Visualizing the Process
Picture this: each night, the liver receives a tiny electric shock (low O₂). The shock lights up fireflies (ROS) inside the cell. Over time, the fireflies multiply, overheating the kitchen and leaving charred spots—those are the fibrotic patches doctors see on imaging.
Who Is at Risk
Overlapping Risk Factors
If you check any of the boxes below, you’re standing at the intersection of two growing epidemics.
Checklist
- Body‑mass index (BMI) ≥ 30 kg/m²
- Loud, chronic snoring or observed pauses in breathing
- Daytime sleepiness or morning headaches
- Elevated liver enzymes (ALT/AST) on routine labs
- High blood pressure, high triglycerides, or type‑2 diabetes
Demographics & Special Groups
Adults over 40 are the classic crowd, but the link shows up in kids too. A 2015 pediatric study found that 60 % of children with fatty liver also had sleep apnea—so if you have an overweight teen who snores, don’t ignore the possibility.
Short Story
Mike, 52, never thought his nightly “snort‑and‑gasp” routine mattered. A routine blood test flagged mildly elevated ALT, and his doctor ordered a sleep study. The results showed an AHI of 31 —moderate OSA. Six months of CPAP plus a Mediterranean diet dropped his ALT by 35 % and shaved 8 kg off his waist.
Getting Diagnosed
When to Ask for a Sleep Study
Ask for a polysomnography if you have any two of the following: loud snoring, witnessed apneas, persistent daytime fatigue, or unexplained liver‑enzyme spikes. Early detection saves both your nights and your liver.
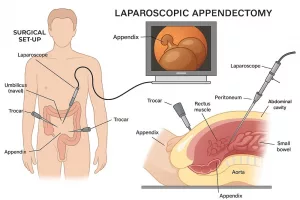
How It Works
A sleep lab wires you to a few sensors: a nasal airflow tube, a chest belt, a pulse‑oximeter, and a microphone for snoring. Over the night the system records breathing patterns and oxygen saturation, delivering an apnea‑hypopnea index (AHI) that grades severity.
Liver Imaging & Labs
For fatty liver, doctors usually start with an abdominal ultrasound—quick, cheap, and decent at spotting steatosis. If the ultrasound is ambiguous or you need fibrosis staging, a FibroScan (transient elastography) is the next step. Blood work typically includes ALT, AST, GGT, fasting lipids, HbA1c, and a complete metabolic panel.
Guideline Reference
According to the American Association for the Study of Liver Diseases (AASLD) guidelines, patients with risk factors for both OSA and MASLD should receive concurrent screening.
Scoring Systems & Combined Risk Algorithms
Physicians often blend the AHI with fibrosis scores like FIB‑4 or the NAFLD fibrosis score (NFS) to gauge overall risk.
Scoring Table
| Metric | Score Range | Interpretation |
|---|---|---|
| AHI (Apnea‑Hypopnea Index) | 0‑5 | Normal |
| AHI | 5‑15 | Mild OSA |
| AHI | 15‑30 | Moderate OSA |
| AHI | >30 | Severe OSA |
| FIB‑4 | <1.3 | Low fibrosis risk |
| FIB‑4 | 1.3‑2.67 | Indeterminate |
| FIB‑4 | >2.67 | High fibrosis risk |
Treatment Options
CPAP First
Continuous Positive Airway Pressure (CPAP) is the gold standard for OSA. By keeping the airway open, CPAP blunts the oxygen dips that fuel liver inflammation. A 2023 meta‑analysis showed a modest but significant reduction in ALT and liver fat fraction after three months of consistent CPAP use.
Adherence Tips (From Experience)
- Start with a mask fitting session—comfort matters more than price.
- Track nightly usage in the device’s app; aim for at least 4 hours per night.
- Keep a sleep‑journal; note energy levels and any liver‑test changes.
Lifestyle & Weight Management
Weight loss is the universal prescription for both conditions. Even a 5 % reduction in body weight can lower AHI by up to 20 % and shrink liver fat by 30 %.
Data Point
Healthline highlighted that patients who combined CPAP with a Mediterranean‑style diet saw the greatest improvement in both sleep quality and liver enzyme profiles.
Pharmacologic Options (MASLD Treatment)
If lifestyle changes aren’t enough, a few meds can tip the scales. GLP‑1 receptor agonists (like semaglutide) improve insulin sensitivity and have been shown to reduce liver fat in clinical trials. Some endocrinologists also prescribe SGLT2 inhibitors for their dual cardio‑renal‑metabolic benefits.
Expert Quote (Suggested)
“In patients with severe OSA and progressive MASLD, adding a GLP‑1 agonist can accelerate weight loss and dampen the inflammatory cascade,” says Dr. Elena Ramirez, hepatology fellow at a major academic center.
Monitoring & Follow‑Up
Because both conditions evolve, a structured follow‑up plan keeps you ahead of the curve.
Follow‑Up Schedule
| Time | What to Check | Who Does It |
|---|---|---|
| 3 months | CPAP compliance, weight, blood pressure | Sleep clinic |
| 6 months | Liver enzymes (ALT/AST), FibroScan | Hepatology |
| 12 months | Full polysomnography if AHI > 15, repeat fibrosis score | Sleep lab |
Myths & Truths
Fatty Liver Causes OSA?
The relationship is mostly one‑way: OSA aggravates fatty liver, but the reverse is less clear. That said, severe liver disease can change hormone levels that affect breathing, so it’s a two‑street but uneven intersection.
CPAP Is a Cure?
CPAP dramatically improves sleep quality and can lower liver enzymes, but it isn’t a standalone cure for MASLD. Weight loss, diet, and sometimes medication remain essential components.
Silent Snorers Need Tests Too
Even if you never hear yourself snore, you can still have obstructive events—especially if you’re overweight or have hypertension. A simple questionnaire (“STOP‑BANG”) can flag hidden apnea.
Real Stories
Anna’s Turnaround
Anna, 45, was diagnosed with moderate OSA (AHI 22) and simple steatosis. After starting CPAP and losing 9 kg through a Mediterranean diet, her ALT dropped 30 % and she no longer felt foggy in the mornings.
Jude’s Journey
Jude, 58, had severe OSA (AHI 48) and fibrosis stage F2. He underwent bariatric surgery, which cut his weight by 25 %. Six months later his AHI fell to 12, and a repeat FibroScan showed regression of fibrosis—a rare but hopeful outcome.
Liam’s Early Wins
Liam, a 13‑year‑old with obesity, was found to have mild OSA and early NAFLD during a school‑based health screen. An oral appliance improved his sleep quality, and a structured after‑school exercise program reduced his liver fat on ultrasound within a year.
Take Action Now
Feeling a little overwhelmed? That’s normal. The key is to pick one step and start today:
- Schedule a sleep study if you have any of the risk factors listed above.
- Ask your primary‑care doctor for a liver ultrasound and basic labs.
- Commit to a 15‑minute walk after dinner—consistency beats intensity.
- If you’re already on CPAP, review the mask fit with your provider; a small adjustment can boost comfort dramatically.
Remember, you’re not alone in this. Millions are navigating the same crossroads, and the medical community is gathering more evidence every day. By staying informed, asking the right questions, and following a balanced plan, you can protect both your nights and your liver.
What’s your experience with sleep‑related breathing issues or liver health? Share in the comments below—your story might help someone else take that first step.
Conclusion
Sleep apnea and fatty liver (MASLD) are tightly linked through intermittent hypoxia, systemic inflammation, insulin resistance, and oxidative stress. The good news is that the same interventions—CPAP, weight loss, a heart‑healthy diet, and targeted medications—can tackle both problems at once. Early screening, personalized treatment, and regular monitoring form the backbone of a successful strategy.
Take a moment right now: jot down any sleep‑related symptoms you notice, schedule that blood test, and consider a gentle walk tonight. Small, consistent actions add up, and before you know it, you’ll be breathing easier and watching your liver health improve. You’ve got this.























Leave a Reply
You must be logged in to post a comment.